Dengue Fever
Background
The World Health Organization (WHO) has declared the ever–worsening threats of global warming and climate change to be new public health challenges. Climate change endangers people's health through natural disasters, such as heat waves and floods, which foster communicable diseases and raise the prevalence of dengue fever. In just the past decade, the significance of dengue as a threat to health and a burden on health services and economies has increased substantially. Compared with the situation 50 years ago, the worldwide incidence of dengue has risen 30–fold. More countries are reporting their first outbreaks. Dengue ranks as the most important mosquito–borne viral disease in the world.
Dengue virus (DENV) is a small single–stranded RNA virus comprising four distinct serotypes (DEN–1 to –4). These closely related serotypes of the dengue virus belong to the genus Flavivirus, family Flaviviridae. The various serotypes of the dengue virus are transmitted to humans through the bites of infected Aedes mosquitoes, principally Ae. aegypti. This mosquito is a species widely distributed in tropical and subtropical regions around the world, mostly between latitudes 35˚N and 35˚S. These geographical limits correspond approximately to a winter isotherm of 10˚C. The immature stages are found in water–filled habitats, mostly in artificial containers closely associated with human dwellings and often indoors. Dengue outbreaks have also been attributed to Aedes albopictus. In recent decades Aedes albopictus has spread from Asia to Africa, the Americas and Europe, notably aided by the international trade in used tyres in which eggs are deposited when they contain rainwater. The eggs can remain viable for many months in the absence of water.
Humans are the main amplifying host of the virus. Dengue virus circulating in the blood of viraemic humans is ingested by female mosquitoes during feeding. The virus then infects the mosquito mid–gut and subsequently spreads systemically over a period of 8–12 days. After this extrinsic incubation period, the virus can be transmitted to other humans during subsequent probing or feeding. The extrinsic incubation period is influenced in part by environmental conditions, especially ambient temperature. Thereafter the mosquito remains infective for the rest of its life. Ae. aegypti is one of the most efficient vectors for arboviruses because it is highly anthropophilic, frequently bites several times before completing oogenesis, and thrives in close proximity to humans.
Dengue begins after an incubation period of 3–14days, usually 4-7days, and has a wide spectrum of clinical presentation, often with unpredictable clinical evolution and outcome. While most patients recover following a self–limiting non–severe clinical course, a small proportion progress to severe disease, mostly characterized by plasma leakage with or without hemorrhage. Intravenous rehydration is the therapy of choice. Appropriate interventions can reduce the case fatality rate to less than 1% of severe cases. The group progressing from non–severe to severe disease is difficult to define. Early diagnosis and prompt supportive treatment can substantially lower the risk of medical complications and death. The most effective protective measures are those that avoid mosquito bites.
Epidemiology
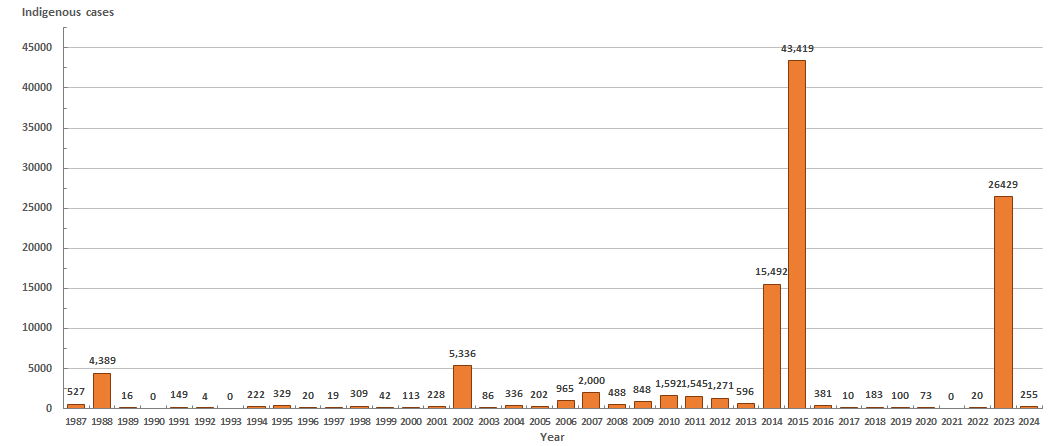
During the first half of the 20th century, there were three island–wide dengue fever outbreaks in Taiwan (1915, 1931, and 1942). After almost forty years of dormancy, a DEN–2 outbreak occurred in Liuchiu Township, Pingtung County in 1981. Thereafter, more dengue fever outbreaks took place in Kaohsiung (1987–1988), Jhonghe of Taipei County (1995), Taichung City (1995), Taipei City (1996) and several others in the Kaohsiung City, Tainan City, and Pingtung County. In 2002, another dengue fever outbreak occurred in southern Taiwan. It was similar to the 1988 outbreak which actually started in 1987. The total number of indigenous cases was 5,336, including 241 cases of dengue hemorrhagic fever (DHF) which caused 19 deaths. After that, the indigenous dengue cases were less than 400 in 2003–2005. Since 2006, Taiwan faced dengue fever outbreaks of different scales every year; the cases were concentrated mainly in southern Taiwan, including Kaohsiung City, Tainan City, and Pingtung County. In 2015, Taiwan battled one of the most severe dengue outbreak in history with over 43,000 dengue cases, including 228 deaths.
The severity of dengue fever in Southeast Asia in recent years has led to an increase in imported cases in Taiwan, with the most 540 cases in 2019. The situation has made it more difficult to control dengue locally.
In response to the COVID-19 pandemic in 2020 to 2022, border controls have been implemented. In 2022, the number of imported cases was 68, the third lowest over the previous 10 years.
After the easing of COVID-19 restrictions in 2023, there was frequent international and domestic exchange, severe epidemics in neighboring Southeast Asian countries, hot and humid climate, and frequent heavy rains. These factors led to a major dengue fever outbreak domestically, with 277 imported cases and 26,429 indigenous cases reported.
Figure: Indigenous dengue cases in Taiwan, 1987-2024.
The World Health Organization (WHO) has declared the ever–worsening threats of global warming and climate change to be new public health challenges. Climate change endangers people's health through natural disasters, such as heat waves and floods, which foster communicable diseases and raise the prevalence of dengue fever. In just the past decade, the significance of dengue as a threat to health and a burden on health services and economies has increased substantially. Compared with the situation 50 years ago, the worldwide incidence of dengue has risen 30–fold. More countries are reporting their first outbreaks. Dengue ranks as the most important mosquito–borne viral disease in the world.
Dengue virus (DENV) is a small single–stranded RNA virus comprising four distinct serotypes (DEN–1 to –4). These closely related serotypes of the dengue virus belong to the genus Flavivirus, family Flaviviridae. The various serotypes of the dengue virus are transmitted to humans through the bites of infected Aedes mosquitoes, principally Ae. aegypti. This mosquito is a species widely distributed in tropical and subtropical regions around the world, mostly between latitudes 35˚N and 35˚S. These geographical limits correspond approximately to a winter isotherm of 10˚C. The immature stages are found in water–filled habitats, mostly in artificial containers closely associated with human dwellings and often indoors. Dengue outbreaks have also been attributed to Aedes albopictus. In recent decades Aedes albopictus has spread from Asia to Africa, the Americas and Europe, notably aided by the international trade in used tyres in which eggs are deposited when they contain rainwater. The eggs can remain viable for many months in the absence of water.
Humans are the main amplifying host of the virus. Dengue virus circulating in the blood of viraemic humans is ingested by female mosquitoes during feeding. The virus then infects the mosquito mid–gut and subsequently spreads systemically over a period of 8–12 days. After this extrinsic incubation period, the virus can be transmitted to other humans during subsequent probing or feeding. The extrinsic incubation period is influenced in part by environmental conditions, especially ambient temperature. Thereafter the mosquito remains infective for the rest of its life. Ae. aegypti is one of the most efficient vectors for arboviruses because it is highly anthropophilic, frequently bites several times before completing oogenesis, and thrives in close proximity to humans.
Dengue begins after an incubation period of 3–14days, usually 4-7days, and has a wide spectrum of clinical presentation, often with unpredictable clinical evolution and outcome. While most patients recover following a self–limiting non–severe clinical course, a small proportion progress to severe disease, mostly characterized by plasma leakage with or without hemorrhage. Intravenous rehydration is the therapy of choice. Appropriate interventions can reduce the case fatality rate to less than 1% of severe cases. The group progressing from non–severe to severe disease is difficult to define. Early diagnosis and prompt supportive treatment can substantially lower the risk of medical complications and death. The most effective protective measures are those that avoid mosquito bites.
Epidemiology
During the first half of the 20th century, there were three island–wide dengue fever outbreaks in Taiwan (1915, 1931, and 1942). After almost forty years of dormancy, a DEN–2 outbreak occurred in Liuchiu Township, Pingtung County in 1981. Thereafter, more dengue fever outbreaks took place in Kaohsiung (1987–1988), Jhonghe of Taipei County (1995), Taichung City (1995), Taipei City (1996) and several others in the Kaohsiung City, Tainan City, and Pingtung County. In 2002, another dengue fever outbreak occurred in southern Taiwan. It was similar to the 1988 outbreak which actually started in 1987. The total number of indigenous cases was 5,336, including 241 cases of dengue hemorrhagic fever (DHF) which caused 19 deaths. After that, the indigenous dengue cases were less than 400 in 2003–2005. Since 2006, Taiwan faced dengue fever outbreaks of different scales every year; the cases were concentrated mainly in southern Taiwan, including Kaohsiung City, Tainan City, and Pingtung County. In 2015, Taiwan battled one of the most severe dengue outbreak in history with over 43,000 dengue cases, including 228 deaths.
The severity of dengue fever in Southeast Asia in recent years has led to an increase in imported cases in Taiwan, with the most 540 cases in 2019. The situation has made it more difficult to control dengue locally.
In response to the COVID-19 pandemic in 2020 to 2022, border controls have been implemented. In 2022, the number of imported cases was 68, the third lowest over the previous 10 years.
After the easing of COVID-19 restrictions in 2023, there was frequent international and domestic exchange, severe epidemics in neighboring Southeast Asian countries, hot and humid climate, and frequent heavy rains. These factors led to a major dengue fever outbreak domestically, with 277 imported cases and 26,429 indigenous cases reported.
Figure: Indigenous dengue cases in Taiwan, 1987-2024.
Figure: Imported dengue cases in Taiwan, 1987-2024.
Dengue Surveillance in Taiwan
- Taiwan National Infectious Disease Statistics System–Dengue Fever
- Fever screening at international airports and seaports.
- Self–reporting through the toll–free 1922 hotline or local public health authority.
Figure: Fever screening at the Taiwan Taoyuan International Airport.

Prevention and Control
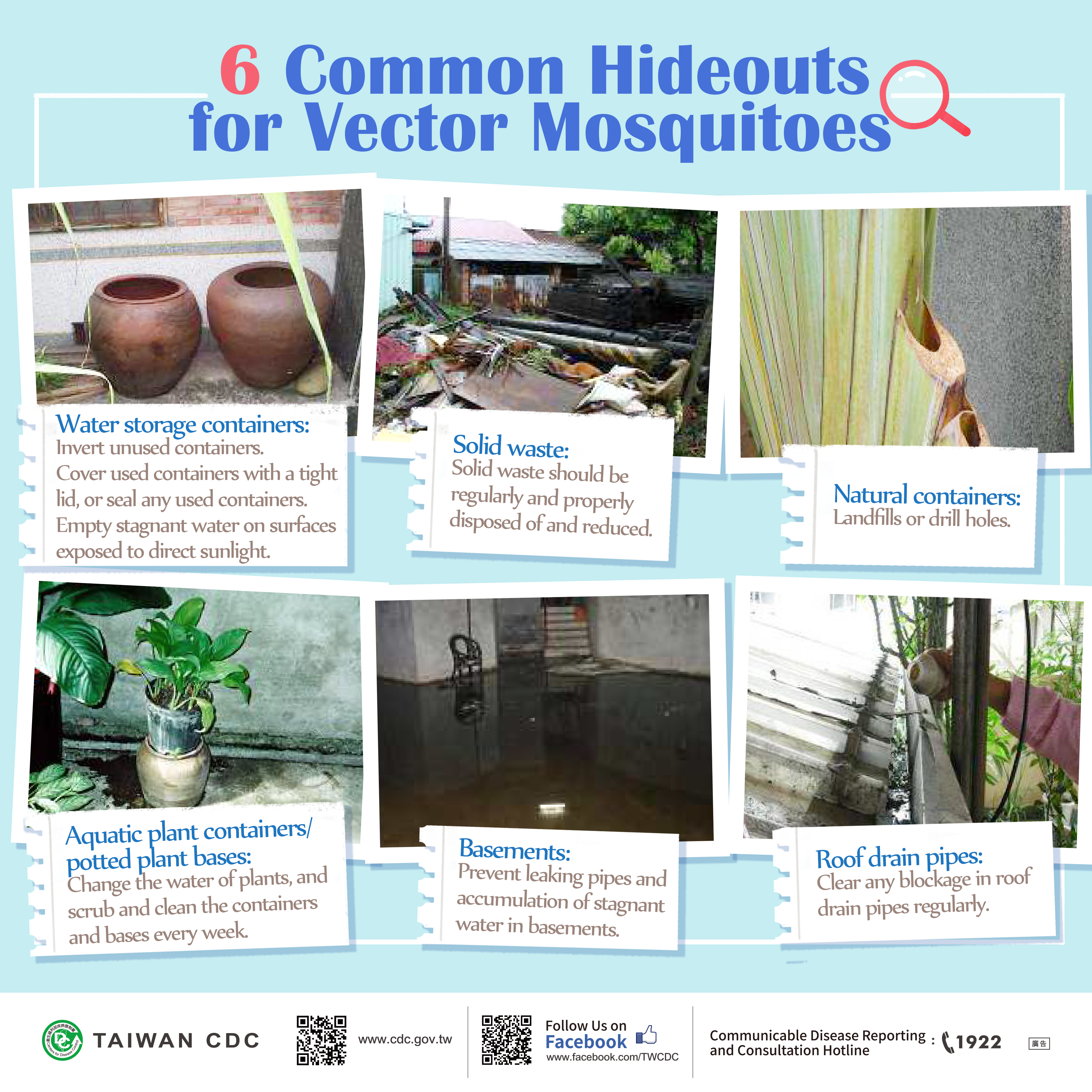
- The main strategies to control dengue fever in Taiwan are eliminating vector breeding sources and effectively lowering vector (mosquito) density.
- Taiwan CDC has devised a three–stage prevention strategy for controlling the dengue fever epidemic.
- (1) Primary prevention measures include source reduction and control of the vector population.
- Implementing health education through various communication channels to promote dengue fever and severe dengue awareness.
- Involving the community in improving environmental and household sanitation along with reducing vector sources through volunteer training.
- Encouraging regular inspection and eliminating vector breeding sources by cleaning empty houses, vacant lots, and other potential vector breeding sources, and keeping a record of these places for future inspections.
- Strengthening education and training for disease prevention workers and volunteers.
- Setting up a vector surveillance mechanism to check places with a high mosquito density probability and promptly wipe out vector sources.
- (2) Secondary measures cover disease surveillance and emergency/contingency mechanisms.
- Constructing a disease surveillance mechanism for prompt control of suspected cases, strengthening disease surveillance and disease trend evaluation through official epidemic reporting systems and emerging disease surveillance, as well as public reporting and symptom declaration forms.
- Setting up emergency/contingency mechanisms to promptly investigate suspected transmission sources and spraying insecticide to eliminate those sources, and publicizing the importance of eliminating vector–breeding sites to prevent possible infection.
- (3) Tertiary prevention involves controlling the mortality rate.
- Establishing guidelines for dengue fever diagnosis and treatment.
- Organizing continuing education workshops for medical personnel to raise health care quality and lower mortality rate.
- (1) Primary prevention measures include source reduction and control of the vector population.
FAQs
- What is dengue fever (DF)?
Dengue fever is an acute viral disease caused by any one of four closely related dengue viruses. The incubation period is 3–14 days, usually 4-7days. Symptoms include high fever, headache, eye pain (behind eyes), muscle and/or joint pain and rash. Generally, younger children have a milder illness than older children and adults. - What is severe dengue?
Severe dengue is a potentially deadly complication due to plasma leaking, fluid accumulation, respiratory distress, severe bleeding, or organ impairment. When developing into severe dengue, the critical phase takes place around 3–7 days after the first sign of illness, and proper medical care is needed to prevent complications and risk of death. - How is dengue fever transmitted?
Dengue is mainly transmitted to people by the bite of mosquito that is infected with the dengue virus. The mosquito becomes infected with dengue virus when it bites a person who has dengue virus in their blood. In Taiwan, the Aedes albopictus and Aedes aegypti mosquito is the most important vector of dengue viruses.There are evidences of the possibility of maternal transmission (from a pregnant mother to her baby)、blood or sexual transmission, while these transmission rates appear low. - What is the treatment for dengue?
There is no specific medication for treatment of a dengue infection. Persons who think they have dengue should use analgesics (pain relievers) with acetaminophen and avoid those containing aspirin. They should also rest, drink plenty of fluids, and consult a physician. - What can be done to reduce the risk of acquiring dengue?
The best preventive measure for residents living in areas infested with Aedes albopictus or Aedes aegypti is to eliminate the places where the mosquito lays eggs, primarily artificial containers that hold water.
(1) Clean and remove any water containers and vector breeding sources.
(2) Always place a tight lid on containers used for water storage.
(3) Weekly, wash out containers with a brush or sponge to remove mosquito eggs.
(4) Wear long sleeve shirts, long pants, socks and closed shoes to avoid mosquito bites.
(5) Use repellents containing DEET (N, N–diethyl–m–toluamide), Picaridin or IR3535 on your clothing and exposed skin.
(6) Use screens on doors and windows.
- WHO|Dengue and severe dengue
- USA CDC|Dengue
- HealthMap|DengueMap
- Dengue Vaccine Initiative (DVI)
- Resources for Prevention, Control and Outbreak Response Dengue:
- (1) Guidelines and Manuals
- (2) Strategies and Best Practices
Images


PublishTime 2014/11/24

