HIV/AIDS
Background
Human Immunodeficiency Virus (HIV) is a virus that infects specific cells of the immune system such as T cells (specifically CD4+ T cells) and causes a lifelong severe illness with a long incubation period. When HIV attacks the immune system and the patients can’t fight off infections and disease, HIV infection leads to acquired immunodeficiency syndrome (AIDS) stage.
HIV can be transmitted by sexual contact (anal sex, oral sex, vaginal sex, etc.), by sharing needles or syringes for drug injection, or through blood transfusions. Also, babies born to HIV-infected women may be infected during birth or through feeding breast milk.
Although there is no effective cure for HIV so far, some effective combination therapies conduct impressive efficiency in prolonging life expectancy of HIV-infected people and even lowering their chance of infecting others. It is important that HIV-infected people receive medical care and treatment as early as possible to have a better prognosis.
Epidemiology
The first HIV case in Taiwan was reported in 1984. As of the end of 2022, the total number of HIV cases had been accumulated to 44,861 (21,294 of whom had developed full-blown AIDS and 8,263 cases had deceased). The number of HIV infections among the injecting drug users (IDUs) began to surge since 2003 and then consistently decreased since Taiwan CDC harm reduction programs. In 2008 and thereafter, the epidemic took a turn; infections mainly occurred through sexual encounter.
Of Taiwanese nationals infected by HIV in 2022, 1207, or 96%, were males and 42, or 4%, were females. The ratio of infected males to females was 25:1. The largest number of infections in 2022 was in the 25 to 39 age group, accounting for 582, or 54%, of all cases. The second largest group was the 40 to 64 age group, numbering 263, or 25%, of all cases. An analysis of risk factors showed that in 2022, the highest proportion of HIV infections was a result of unsafe sexual transmission, with men who have sex with men (MSM) accounting for 80% of all cases. The second largest proportion of infections was heterosexual contact, accounting for 11%. (see Figure 1).
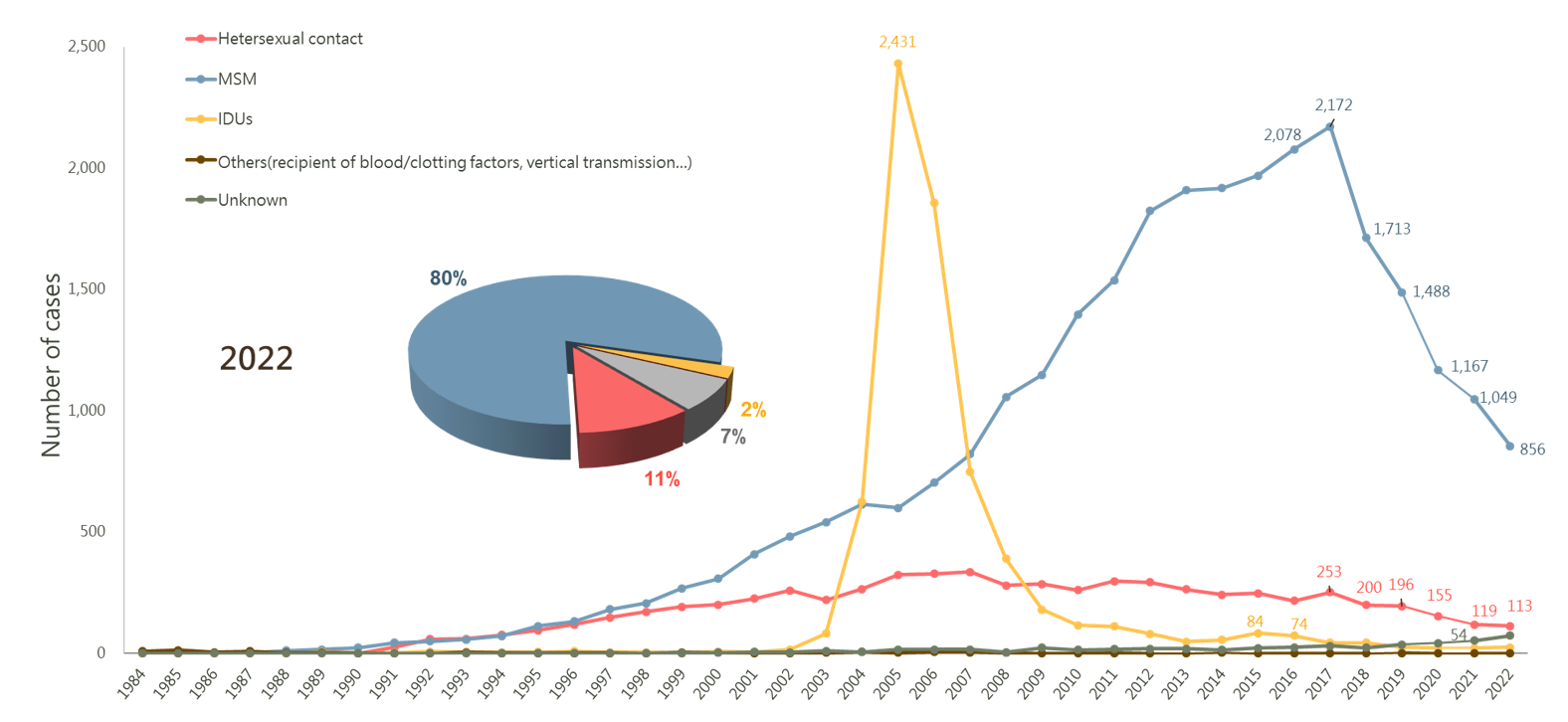
Statistics on Risk Factors of HIV Infections in Taiwan, 1984-2022
Figure 1: Statistics on Risk Factors of HIV Infections in Taiwan, 1984-2022
Prevention and Control
- Reducing the number of new HIV infections.
- Promoting apposite HIV prevention educations and policy for different vulnerable groups.
- Implementing National Pre-Exposure Prophylaxis (PrEP) program.
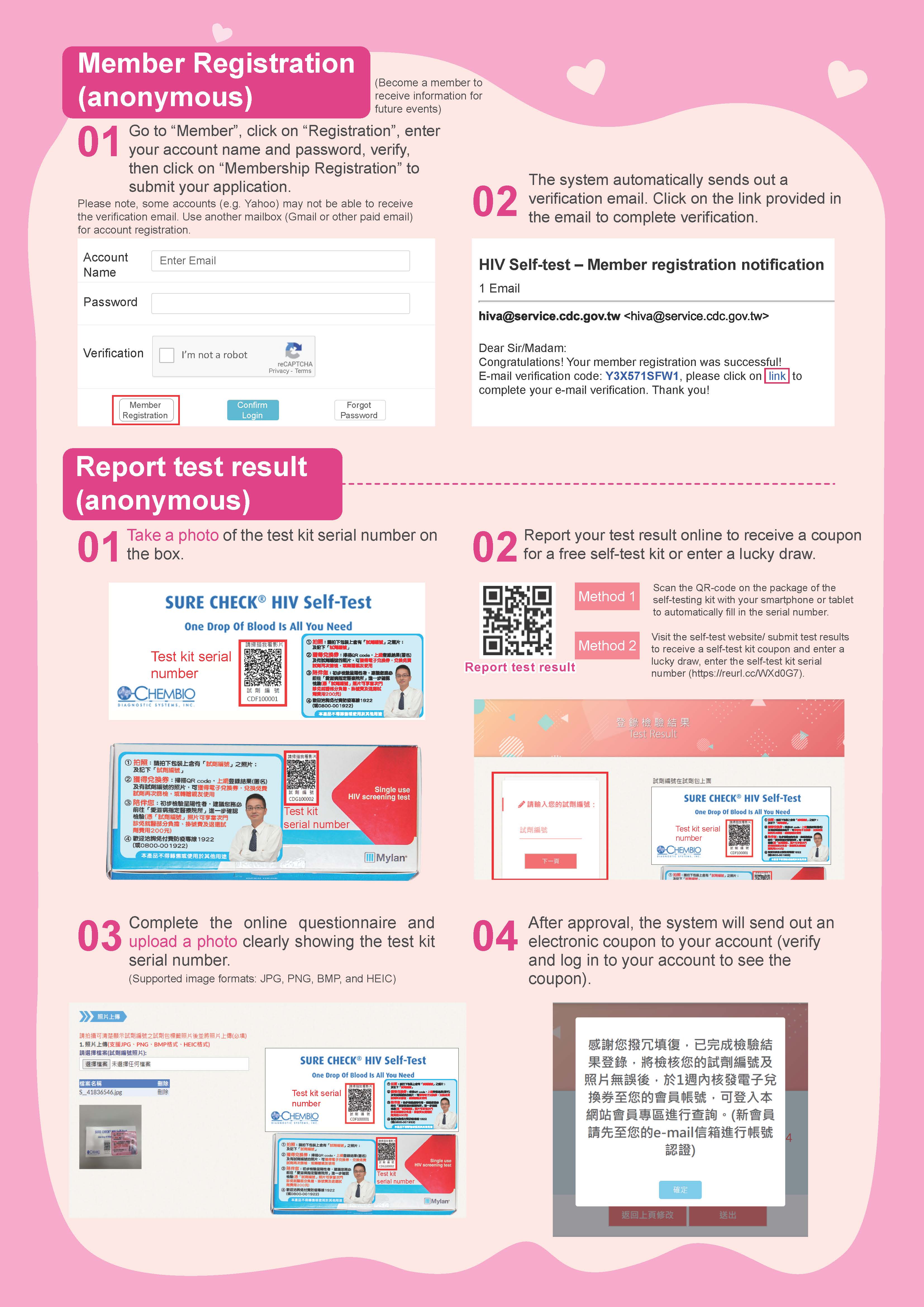
- Developing multiple programs for HIV testing, consultation and referral services. (e.g. Implementing HIV self-test program which allows people to order HIV self-test kits online, then pay and pickup the kits at chained convenient stores.)
- Post-exposure Prophylaxis (PEP) for occupational and non-occupational exposure to HIV. Regarding the occupational PEP (oPEP), CDC provides subsidies for medication and HIV testing.
- Encouraging doctors to participate in sexual health friendly clinics program.
- Expanding universal access to antiretroviral therapy for people living with HIV who need it.
- Advancing of essential care and ongoing support for people living with HIV.
- Optimizing HIV related laws and regulations.
FAQ
- What are HIV and AIDS?
- AIDS, also known as acquired immunodeficiency syndrome; referred to AIDS is a disease caused by the HIV, which violated the human immune system. People infected by HIV usually do not immediately lead to AIDS. At first, one may not have any symptoms or get sick during the phase of immunity gap. Without treatment, HIV will continuously attack the immune system, so the infected person gradually lose immunity, and even death.
- How is HIV transmitted?
- Only certain fluids—blood, semen (cum), pre-seminal fluid (pre-cum), rectal fluids, vaginal fluids, and breast milk—from an HIV-infected person can transmit HIV.
- In Taiwan, HIV is spread mainly by having unprotected sex (e.g. without using condoms and lubricants), including anal sex, vaginal sex. Less commonly, HIV may be spread by mother-to-child transmission, blood transfusion and hemophiliacs.
- What is the Pre-Exposure Prophylaxis (PrEP) for HIV prevention?
- PrEP is an HIV prevention strategy recommended by World Health Organization (WHO). It is a medication that users take daily (or on-demand for men who have sex with men, MSM) to prevent themselves from getting HIV. Studies showed that taking PrEP as a prescription reduces the risk of infecting by HIV via sexual contact by more than 90% and by at least 74% through drug injection. However, it doesn’t protect one from getting another sexually transmitted disease (STD). Therefore, using condoms and lubricants while having sex is highly recommended.
- Who should consider using PrEP?
- Sexually-active people who are HIV negative.
- People who inject drugs.
- Having regular sex partner who has been diagnosed with HIV.
- Having unprotected sex (without using condoms and lubricants).
- If you are the spouse or the partner of Taiwanese, you can join the government funded PrEP program; otherwise you can pay out-of-pocket, Click here to view the List.
- How to take PrEP?
- Daily PrEP: Daily PrEP (taking one pill once a day, every day) is recommended for female, sexually-active people and people who inject drugs.
- On-demand PrEP: On-demand PrEP is only for MSM or bisexual men. It involves taking two pills 2-24 hours before possible sexual exposure to HIV and then continuing to take one pill each day until two days after their last possible sexual exposure. The effect of on-demand PrEP for heterosexual men, women, people who inject drugs, and transgender has not yet been discovered.
- Can adolescents take PrEP?
- Yes. PrEP pills are approved and can be used by adolescents who are HIV negative, weigh at least 35 kg, and are at risk of getting HIV from sex or drug injection.
- Should I get tested for HIV?
- Everyone who had sex before should get tested for HIV at least once.
- If you have unprotected sex (without using condoms and lubricants), then you should get tested at least once a year.
- Sexually active people and those who have higher risk of getting HIV (e.g. sharing needles, syringes or other equipment to inject drugs, having multiple sexual partners, having addiction to use drugs during sex, and being diagnosed with another STD) should get tested every 3 to 6 months.
- Where can I get HIV tested?
- You can ask your health care provider for an HIV test. Many medical institutions, including clinics and hospitals, provide anonymous HIV testing and counselling services as well. To make HIV testing more accessible, the local health bureaus, the LGBTI+ friendly community health centers and some NGOs offer the outreach HIV testing services in different occasions, such as gyms, parties, bars, saunas, etc. You can also buy a HIV self-test kit through community service sites, vending machines, or order it online then pick-up at your nearby convenient stores.
Click here to view the information of testing.
1.anonymous HIV testing and counselling services
2.HIV self-test
- You can ask your health care provider for an HIV test. Many medical institutions, including clinics and hospitals, provide anonymous HIV testing and counselling services as well. To make HIV testing more accessible, the local health bureaus, the LGBTI+ friendly community health centers and some NGOs offer the outreach HIV testing services in different occasions, such as gyms, parties, bars, saunas, etc. You can also buy a HIV self-test kit through community service sites, vending machines, or order it online then pick-up at your nearby convenient stores.
- What is the Post-Exposure Prophylaxis (PEP) for HIV?
- Post-Exposure Prophylaxis (PEP) is the use of antiretroviral drugs after a single high-risk event to stop HIV from making copies of itself and spreading through your body. PEP must be started as soon as possible to be effective—and always within 3 days(72 hours) of a possible exposure.
- When should I get PEP ?
- If you think you may have been exposed to HIV very recently, see a doctor as soon as possible to find out if PEP is right for you.
- Where can I get sexual health friendly service?
- There are several clinics and hospitals provide sexual health services, including consultation of HIV and other STDs and referral services. Click here to view the List.
- If I am HIV-positive, where can get the medical care?
- There are many designated hospitals and clinics provide medical care for HIV/AIDS patients around Taiwan. Click here to view the List.
- What is the treatment for HIV/AIDS?
- There is no cure for HIV infection so far. Nevertheless, there are various treatment options that can help people living with HIV experience long and productive lives. In Taiwan, domestic government has provided free medical treatment and free highly active antiretroviral therapy (HAART or ART) to the HIV/AIDS patients. The patients are given various free antiretroviral drugs after diagnosis.
- If you are a foreigner,please refer to Foreigner with HIV infection in Taiwan: Question and Answer. Click here to view the List.
More Information
- UNAIDS
- WHO
- Virtual AIDS office of Hong Kong
- STI Online - Sexually Transmitted Infections (Sexually Transmitted Infections) Online
- AIDS Prevention Information Network
- AIDS info
- National minority AIDS council
- UCSF AIDS Health Project
- Asian and Pacific Islander Coalition
- HIV InSite Gateway to HIV and AIDS Knowledge
- AVERT - A UK HIV and AIDS Charity
- The Global Fund to fight AIDS, Tuberculosis and Malaria
- Foreigner with human immunodeficiency viruses (HIV) infection in Taiwan: Question and Answer
Images