Tuberculosis
Background
Tuberculosis (TB)
- Tuberculosis is an airborne infectious disease caused by bacteria (usually Mycobacterium Tuberculosis (MTB)). TB bacteria contained in body secretion are put into the air when an infectious TB patient coughs, sneezes, speaks, or sings. Healthy people nearby TB patients may breathe in these bacteria and become infected. The incubation period of the bacteria is estimated to be between 4 and 12 weeks. TB bacteria typically attack lungs, but can also invade other organs and tissues of the body, such as lymph nodes, meninges, pleura, kidney, bone, skin, gastrointestinal tract, urogenital tract, etc.
- Not everyone infected with TB bacteria will develop TB. Generally, they are under control and will not develop TB when host’s immunity is strong enough. Such state of balance is called latent TB infection (LTBI). However, TB may develop when their immune system become weak. Therefore, family members of infectious TB patient, elderly, people with diabetes, silicosis, renal dialysis patients, long-term users of steroids, other immunosuppressive drugs users, alcoholics, and immunocompromised individuals are more likely to develop TB.
- According to the researches, people infected with TB bacteria have a 10% risk of falling ill with TB. Treating TB is necessary to TB patients, and most of the patients can be cured with proper treatment. On the contrary, 50% of the patients will die if they do not receive treatment. Although 30% of patients will survive, they will continue to disseminate bacteria and infect people who are in close contact with them, which may cause more infected cases and place a large financial burden on themselves and society.
- Furthermore, when TB patients do not take medication regularly, the bacteria in their body will develop resistance to the drugs, such that the commonly used anti-TB drugs will become ineffective. Drug resistant TB (DR-TB) is spread the same wat that drug-susceptible TB is spread. For DR-TB patients, especially in multi-drug resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) situation, they need to face with more difficulties to recover, and might need to be detained in hospitals if they failed comply with the treatment according to the Communicable Disease Control Act.
- When TB bacteria enter human body, they form an organized structure called granuloma in the lung. Generally, they are under control and will not develop TB when host’s immunity is strong enough. Such state of balance is called latent TB infection (LTBI). Although LTBI individuals are asymptomatic and not contagious, they may develop TB when their immune system become weak, and symptoms include coughing with or without sputum over 2 weeks, hemoptysis, night sweats, poor appetite, weight loss, chronic fatigue and discomfort, mild fever, chest tightness and pain might occur. Please stay vigilant when symptoms occur, and wear a medical mask properly then consult a doctor to receive TB examinations.
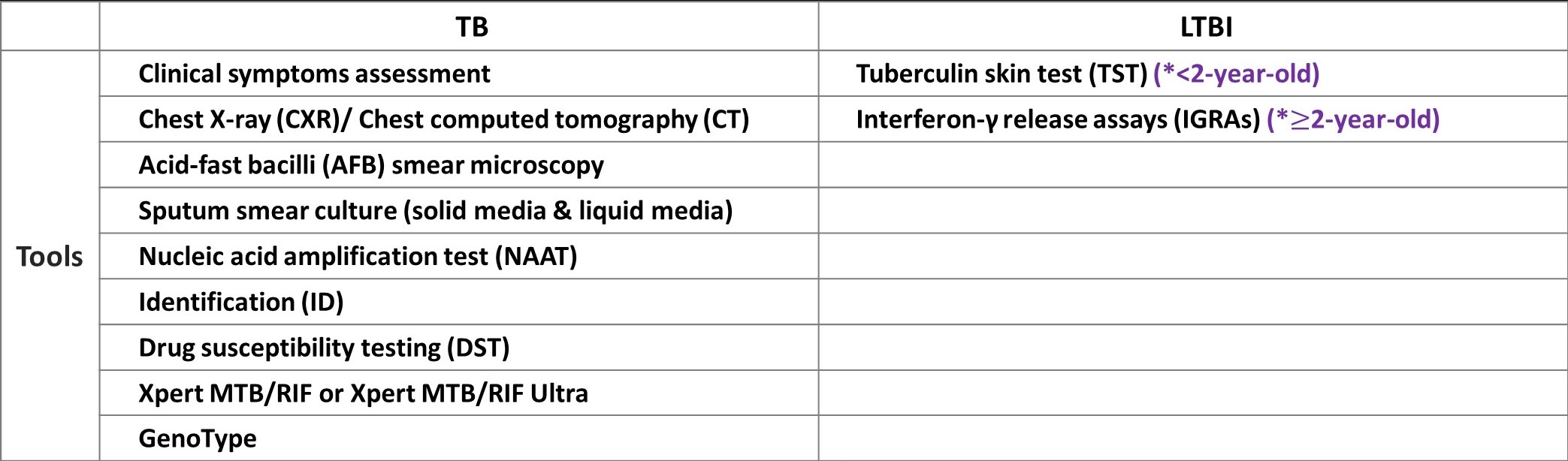
- To prevent LTBI individuals develop TB disease, diagnosis and treatment are critical. Two tests, Interferon-γ release assays (IGRAs) and Tuberculin skin test (TST), are available for different ages of target. For people who have ever been in contact with contagious TB cases, public health authorities will refer them to receive chest X-ray and LTBI test. Receiving the completed course of LTBI treatment provides efficacy over 90% to prevent the subsequent development of TB.
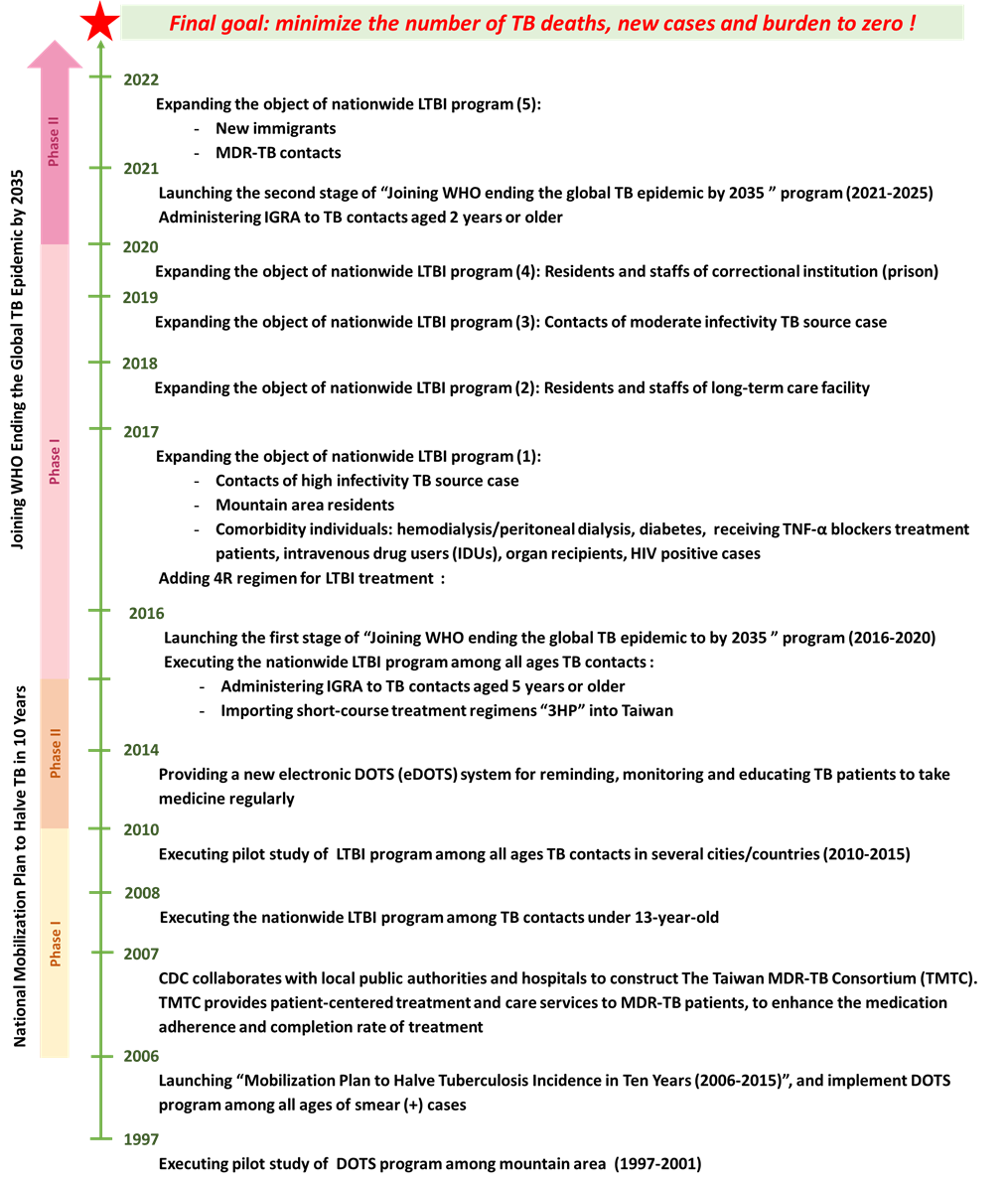
- TB patients are recommended to join the “Directly observed therapy (DOTS)” program, and LTBI individuals should join the “Directly Observed Preventive Treatment (DOPT)” program provided by public health authority, where a trained caregiver (e.g., DOTS/DOPT worker) will provide individual care and medication service. DOTS/DOPT workers ensure patients/individuals take every prescribed pill of the medication regularly, provide care and support, evaluate discomforts or side effects derived from the medication so as to help patients/cases complete the treatment.
Epidemiology
Tuberculosis is one of the most widespread communicable diseases in the world. In 2020, World Health Organization (WHO) estimates that there were 10 million incident TB cases, 1.5 million TB deaths, being the second leading infectious killer after COVID-19.
As for Taiwan, there were 6,576 tuberculosis cases (28 cases per 100,000 population) and 477 tuberculosis-related deaths (2 cases per 100,000 population) in 2022. Obviously, the incidence rate has been showing a continuous downward trend.

Prevention and Control
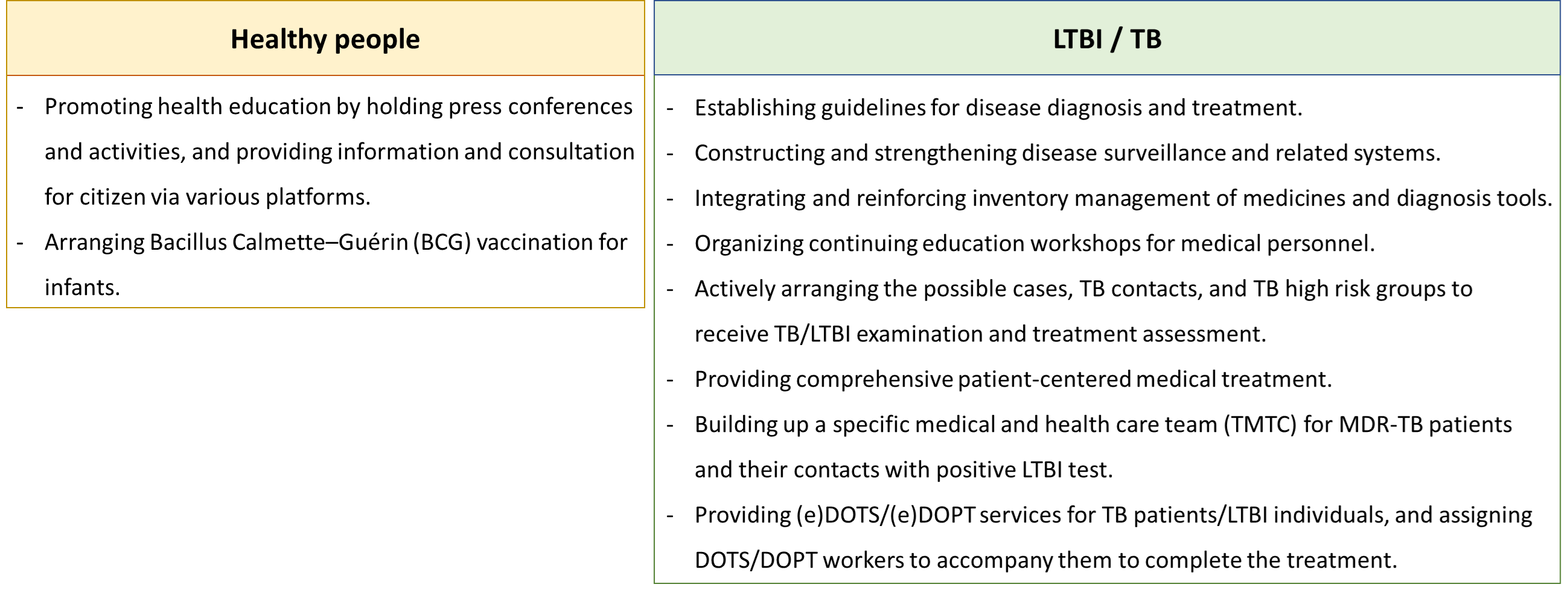
Important TB/LTBI policies and strategies in Taiwan
FAQs
- What is TB/LTBI?
- Tuberculosis transmits when people breathe in air contaminated by droplets and small airborne particles containing the bacteria. Usually, people get infection will not develop TB when host’s immunity is strong enough, such cases are known as latent tuberculosis infection (LTBI). LTBI individuals are asymptomatic and not contagious. However, TB may develop when their immune system become weak, and TB bacteria may further invade lungs and other parts of the body. It can be fatal if TB patients do not receive treatment timely or properly.
- Is there any vaccine that can act as a prevention measure?
- Yes. Bacillus Calmette-Guérin (BCG) is a vaccine against severe tuberculosis (TB) in young children. Research shows that the incidence rate of tuberculous meningitis among young children without BCG vaccinated is 152 cases per million population. In the absence of early intervention, tuberculous meningitis will cause irreversible cerebrospinal disorders (e.g., loss of selfcare ability and intelligence impairment ) and accompany with a case fatality rate up to 20-40%. Infants are recommended to get vaccinated during 5-8 months after birth or no later than one year old. Besides, infants live in areas at particularly high incidence rate or plan to leave for countries with high TB incidence rate should get vaccinated earlier.
- Is there any signs that I can beware of TB development?
- At the early stage of the development of TB disease, symptoms may not be obvious due to the individual’s immunity. Signs and symptoms of TB include coughing with or without sputum over 2 weeks, hemoptysis, night sweats, poor appetite, weight loss, chronic fatigue and discomfort, mild fever, chest tightness and pain.
- What should I do when symptoms occur?
- While TB symptoms occur, you should wear a medical mask properly then consult a doctor to receive TB examinations. Do not worry or hesitate to receive treatment when the positive result confirmed. There are effective medicines for TB, and most of the patients can be cured with proper treatment.
- What is drug-resistant tuberculosis (DR-TB)?
- When TB patients do not take medication regularly, the bacteria in their body will develop resistance to the drugs, such that the commonly used anti-TB drugs will become ineffective. When other healthy people get infected with resistant TB bacteria, DR-TB will develop. Moreover, multidrug-resistant tuberculosis (MDR-TB) development is caused by TB bacteria that are resistant to at least isoniazid and rifampin, the two most potent TB drugs. Since the commonly-used anti-TB drugs are not effective for DR-TB, it is necessary to switch to second-line drugs treatment. However, second-line drugs are more likely to cause gastrointestinal discomforts and are less effective. Therefore, the course of treatment has to be extended and lessen the cure rate, and increase the possibility of becoming XDR-TB patients.
- What is the DOTS/DOPT?
- DOTS stands for “Directly Observed Treatment, Short Course”, and DOPT stands for “Directly Observed Preventive Treatment (DOPT)”. DOTS is applicable to TB patients, and DOPT is suitable for LTBI individuals. The purpose of these programs are to ensure TB patients/LTBI individuals take every prescribed pill of the medication regularly under the intensive care of the healthcare staffs or caregivers (namely DOTS/DOPT workers). To facilitate individuals complete the full course of treatment, healthcare staffs or DOTS/DOPT workers also provide care and support, and help to monitor discomforts or side effects. It is the most effective approach that not only minimizes the side effects of the medication, but also protects the general public by preventing the spread of the disease.
- Can migrant workers diagnosed with tuberculosis or tuberculosis pleurisy receive treatment in Taiwan ?
- Migrant workers diagnosed with tuberculosis or tuberculosis pleurisy (excluding multidrug-resistant tuberculosis (MDR-TB)) can receive treatment in Taiwan and retain right to work after complete the following process. Firstly, they need to sign the approval of “Directly Observed Treatment, Short Course (DOTS) Consent form for Foreign Employee”, and employers should submit the application documents to local health departments. Nevertheless, if migrant workers do not follow DOTS program more than 15 days, or are diagnosed with MDR-TB in subsequent tests, their health examination are regarded as failed, and their “Permit(s) to employ Foreign Worker” will be abolished and workers should be repatriated. As a consequence, migrant workers are ill with tuberculosis or tuberculosis pleurisy should join DOTS and complete TB treatment, so as to protect their rights to health and work. For more details, please check Workforce Development Agency, Ministry of Labor (WDA) website.
https://daily.cdc.gov.tw/Care_EN.html
Related Associations and Institutions
Domestic
- Taiwan Society of Tuberculosis and Lung diseases (台灣結核暨肺部疾病醫學會)
- Taiwan Anti-Tuberculosis Association (中華民國防癆協會)
- Taiwan Society of Pulmonary and Critical Care Medicine (台灣胸腔暨重症加護醫學會)
- Taiwan Society of Pediatric Pulmonology and Critical Care Medicine
- Pediatric Infectious Diseases Society of Taiwan (台灣兒童感染症醫學會)
- The infectious Disease Society of Taiwan (台灣感染症醫學會)
- Taiwan Association of Family Medicine (台灣家庭醫學醫學會)
- Taiwan Pediatric Association (臺灣兒科醫學會)
- International Union Against Tuberculosis and Lung Disease(IUATLD)
- The Global Fund to Fight AIDS, Tuberculosis and Malaria
- Stop TB Partnership
- CDC-Division of Tuberculosis Elimination
發佈日期 2017/1/1

